Ontario Renal Plan 3 2019–2023
The release of the third Ontario Renal Plan coincides with the Ontario Renal Network’s tenth anniversary. Over the past decade, there have been significant improvements in the way kidney care services are delivered and managed in the province. This plan builds on that progress and will continue under Ontario Health.
Ontario Health is a single agency that will, in time, take on the Ontario Renal Network’s work as part of Ontario Health’s larger mandate to oversee healthcare delivery in Ontario, improve clinical guidance and support providers to ensure better quality care for patients.
Working together, we[*] will achieve our common goal to create a system that delivers person-centred, safe and effective kidney care services in an efficient, equitable and timely manner.
Goals & Strategic Objectives
Person-centred
Partner with patients and caregivers to strengthen an inclusive kidney care system
Safe
Empower patients, caregivers and healthcare professionals to reduce avoidable harm
Equitable
Enable responsive and respectful kidney care for patients, regardless of who they are or where they live
Efficient
Improve the efficiency and coordination of the kidney care system
Effective
Deliver kidney care using best evidence
Timely
Improve patients’ access to the care they need
Chronic Kidney Disease in Ontario
Why Ontario needs a renal plan
Almost 12,000 Ontarians with advanced chronic kidney disease require dialysis. An additional 10,000 people in Ontario have advanced chronic kidney disease and receive care from multi-care kidney clinics.[*]
Living with this disease can present tremendous challenges to patients and their caregivers. Depending on the stage of disease and treatment, they may have to deal with:
- significant physical discomfort
- emotional distress
- financial difficulties
- major lifestyle changes
The Ontario Renal Plan shows patients, caregivers and healthcare professionals there is a system dedicated to partnering with them to make continual improvement over the long term.
Kidney disease trends
When a person’s kidneys stop working, dialysis or a kidney transplant may be required to replace kidney function.
Nearly 12,000 people in Ontario receive dialysis.[*]
The number of people on dialysis has grown by an average of 2.3% per year in recent years.
Number of people receiving chronic dialysis, 2015 to 2018[*]
- 2018: 11,610
- 2017: 11,316
- 2016: 11,179
- 2015: 10,836
Several factors are driving an increased need for kidney care, including dialysis.
- Growing population: In 2017, Ontario was home to more than 14 million people. By 2041, our population is projected to grow to 20 million.[*]
- Aging: Chronic kidney disease is more common in the later years of life. Seniors ages 65 and older now represent about 17% of Ontario’s population. This is expected to rise to more than 24% by 2041.[*]
- Diabetes: Diabetes is the most common cause of chronic kidney disease. About 1.6 million Ontarians, representing over 10% of the provincial population, are living with diabetes.[*]
- Hypertension: High blood pressure increases the risk of getting kidney disease and of making it worse. More than 2 million Ontarians have high blood pressure – about 18% of the population.[*]
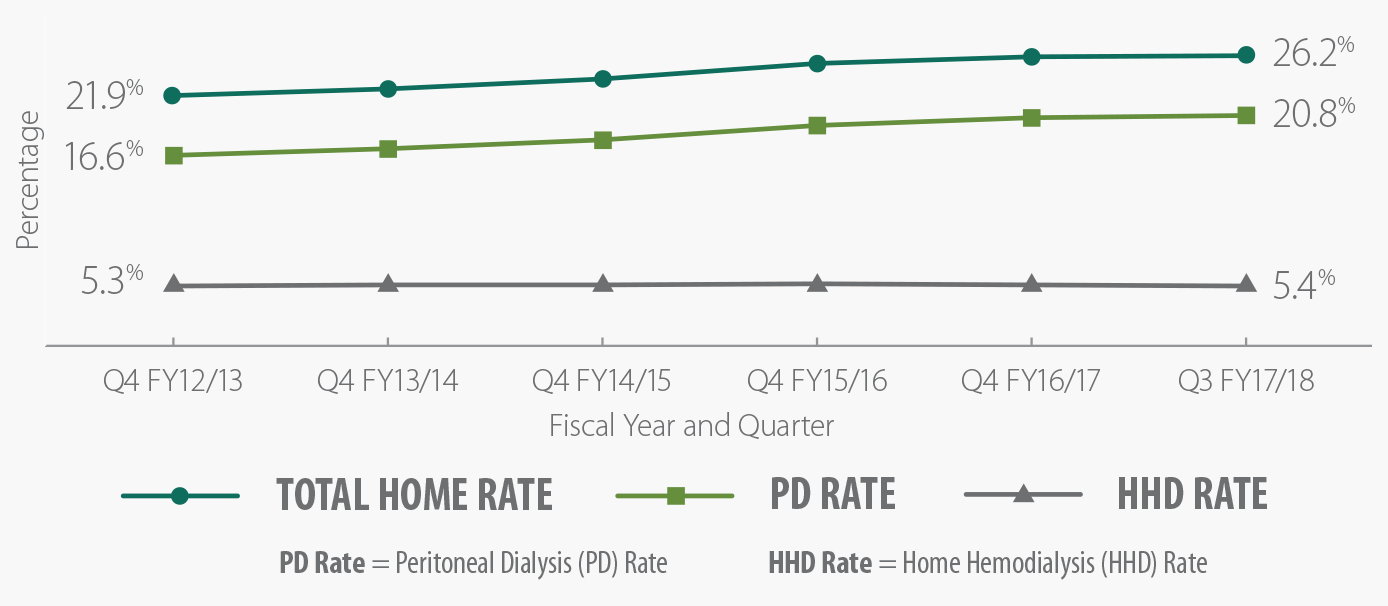
The rate of home dialysis is increasing steadily
Dialysis at home has been shown to improve outcomes, quality of life and independence for patients who choose dialysis as their treatment option. Over the past 4 years, efforts have been made across the Ontario Renal Network to support patients who wish to dialyze at home, and there has been an increase to the rate of home dialysis across Ontario.
More kidney transplants are needed
Kidney transplantation, especially from a living donor, provides the best long-term outcomes for people with end-stage kidney disease. People who have a transplant have a better quality of life and a reduced risk of dying from kidney disease. However, donor organs remain limited and recipients wait a long time for a transplant.
In Ontario, deceased donor kidney transplants have been growing, with the highest number on record achieved in 2017. Living donor transplant numbers have remained static for the past few years.
Strategies to increase access to living kidney donor transplants give people the opportunity to get the best available treatment for end-stage kidney disease.
Chronic kidney disease does not affect everyone in the province equally
Some groups of people in Ontario are at higher risk for developing the disease and face greater challenges in receiving care.
Compared with other Canadians, First Nations, Inuit, Métis and urban Indigenous people are more than 3 times as likely to need treatment for end-stage kidney disease. On average, they must travel 4 times the distance to receive treatment.
The Ontario Renal Plan provides a road map for the way we will work together to reduce the burden of chronic kidney disease on people and the health system.
For more information
Ontario Renal Reporting System
The Ontario Renal Reporting System is a foundational system used to capture data on multi-care kidney clinics, acute dialysis and chronic dialysis in the province. This data is essential to improving system quality, performance, planning and funding.
Trillium Gift of Life Network
Trillium Gift of Life Network is the provincial government agency responsible for planning, promoting, coordinating and supporting organ and tissue donation and transplantation across the province.
In time, the work of Trillium Gift of Life Network will be taken on by Ontario Health. Ontario Health is a single agency that will oversee healthcare delivery in Ontario, improve clinical guidance and support providers to ensure better quality care for patients.
Our Network
Putting the Ontario Renal Plan into action
Developing and implementing the Ontario Renal Plan involves the collaborative efforts of many individuals across all areas of the kidney care system. From patients and their caregivers, nephrologists, Regional Renal Programs and partners, to provincial renal offices and the Ministry of Health and Long-Term Care, we[*] all share a commitment to improving the quality, experience and outcome of care for people affected by chronic kidney disease.
Person-centred care
Patient and family engagement is the cornerstone of the person-centred approach to our work. People with chronic kidney disease and their caregivers offer unique perspectives on the healthcare system.
Thank you to the more than 100 patients and caregivers from across the province who shared their views about the kidney care system and helped guide the development of the Ontario Renal Plan. Their experiences and advice were vital in creating a plan that addresses the diverse needs and values of the populations we serve.
Regional Renal Programs
The Regional Renal Programs are especially important in the collective work to improve the quality and delivery of kidney care services. They use the Ontario Renal Plan to guide their work at the local level. Together with their local Patient and Family Advisory Councils, Local Health Integration Networks (which will, in time, transition to Ontario Health and Ontario Health Teams) and long-term care homes, the Regional Renal Programs make sure people across Ontario can access high-quality kidney care services as close to home as possible.
It is at the local level that dedicated front-line healthcare professionals and behind-the-scenes program administrators implement the improvements in care described in this plan.

“For a frontline worker such as myself, a provincial renal plan provides a structure to build an individualized care plan for each patient I come into contact with. The work that comes out of the Ontario Renal Plan provides me with the best practice guidelines, data reports and processes that guide the care I deliver. With a clear view of the big picture, I can focus on what matters: the patient in front of me.”
Adrienne Barrett
Dialysis Access/Independent Dialysis Registered Nurse
Health Sciences North Horizon Santé-Nord
Recipient of a 2018 Human Touch Award
Medical leadership
Provincial and Regional Medical Leads provide leadership and expert advice to help improve the kidney care system. The Ontario Renal Network’s Medical Leads, who are primarily nephrologists, participate on expert panels and advisory committees, and as reviewers to support our work including the development of guidelines and other evidence-based clinical tools and educational information. With their expertise, we translate knowledge and evidence into planning, policy and program design recommendations and decisions across the kidney care journey. Their contributions are essential to achieving our goals.
Working with the government
The Ministry of Health and Long-Term Care reviews and assesses the Ontario Renal Plan and provides funding for its programs and projects. We advise the ministry about the kidney care system and regularly report on the results of our work.
For more information
Regional Renal Programs
The Regional Renal Programs in Ontario bring together the healthcare organizations and professionals who provide kidney care services within the regions.
Patient and Family Advisors
Dozens of patient and family advisors worked with all areas of the Ontario Renal Network. As policies, programs and practices are developed to meet the goals of the Ontario Renal Plan, their input will help shape decisions that affect patient care and services.
Measuring Progress
Accountability and measurement
We[*] are accountable to the Ministry of Health and Long-Term Care, our network and the people of Ontario for meeting the commitments outlined in this plan.
An annual business plan submitted to the ministry and a detailed internal operating plan set out how we will work with renal system partners to develop and put in place projects and programs to support the plan’s goals and strategic objectives.
There is a robust measurement plan, including performance indicators, to measure progress.
Progress will be reported in several ways:
- Annual report
- Quarterly and special program reports
- Quarterly reports on our accountability and funding agreements
All of this information is used to adjust planning and respond to changes.

Progress to date
This Ontario Renal Plan was built on the achievements of our previous plans.
The inaugural Ontario Renal Plan, 2012 to 2015, addressed the detection, diagnosis and treatment of chronic kidney disease in a systematic way for the first time in this province’s history.
The second Ontario Renal Plan, 2015 to 2019, continued to strengthen the kidney care system with a focus on patient engagement, integration of care and access to care.
Measuring and reporting progress helped to identify areas in which work needs to continue to achieve the goals of the plan.
Read more about the Ontario Renal Network’s second Ontario Renal Plan 2015- 2019.
For more information
CCO’s Governance Documents
CCO’s annual report includes performance targets and reports for the Ontario Renal Network. The annual business plan maps out a strategic direction and activities for the next 3 fiscal years.
About this plan
The Ontario Renal Plan is a road map for the way we[*] will work together with Regional Renal Programs, nephrologists, patient and family advisors, partners and the provincial government to develop and deliver kidney care services through to 2023.
The goals and strategic objectives in the plan help to:
- ensure patients and their caregivers are partners in their care
- identify priorities to guide our work at all levels
- focus our efforts where they are most needed
- advise the government on major initiatives and funding decisions
- develop program-level strategic plans
- bring together many partners within our complex health system
Developing the plan
The Ontario Renal Network began by reviewing the performance of the kidney care system and progress made under the previous plan (2015 to 2019).
We also consulted with more than 450 people from our network, including the Regional Renal Programs, nephrologists, partners, patients and caregivers (including patient and family advisors from the Regional Renal Programs). We are grateful for their insights and expertise.
This information helped us understand how patients and caregivers experience their care, the system’s strengths and opportunities for improvement.
For more information
CCO Health
The Ontario Renal Network is a division of CCO, an agency of the Ministry of Health and Long-Term Care. CCO leads multi-year planning for the cancer system, kidney care system and access to care for key health services.
A single agency named Ontario Health will in time take on CCO’s work as part of Ontario Health’s larger mandate to oversee healthcare delivery in Ontario, improve clinical guidance and support providers to ensure better quality care for patients.